Meningioma
Another of the most common brain tumors is the meningioma. Meningiomas account for 35% of all primary brain tumors. They are usually benign, although there is a more aggressive atypical variant as well as a very unusual malignant version. These have been graded by the World Health Organization as WHO Grades I, II, and III respectively. There are times that meningiomas arise in a very difficult place that may render them difficult or impossible to completely resect.
Meningiomas arise from arachnoid cap cells that are found in one of the lining membranes surrounding the brain. These tumors grow from outside the brain, and as they enlarge, they compress the adjacent brain. Because they usually grow slowly, they often reach very large sizes before symptoms and signs of brain compression occur.
Meningiomas are frequently associated with an abnormality of chromosome 22. They may also be prone to grow more during pregnancy and may have estrogen and progesterone receptors. Previous radiation to the head can be a risk factor.
Sometimes your doctor may choose to simply watch your meningioma because some grow very slowly. Therefore if the patient is of an advanced age or is too medically fragile for surgery, not treating the meningioma may be viewed as a reasonable strategy. However, in general these tumors will grow over time, and a reasonable argument can be made for removing them when they are small before they involve critical structures that could make a delayed removal more dangerous and more time-consuming. Therefore, depending on a meningioma's size, location, and demonstrated rate of growth, treatment is often a more pragmatic strategy than merely observation with serial imaging.
Surgical resection (if complete) will cure a meningioma. If one living cell is left behind, it could recur. Ongoing imaging surveillance is therefore reasonable after surgical removal. If a meningioma cannot be removed completely because its growth is incorporated with important structures such as nerves, arteries, or important veins, then sometimes a strategy of partial resection, followed by serial imaging and follow up will be used. Alternatively, a combined treatment strategy might be used that includes radiation or stereotactic radiosurgery (which is not really surgery but a form of high dose radiation delivered with the aid of a computer and a stereotactic frame that is applied by the neurosurgeon to the patient). In some cases, a meningioma may be treated only with radiation or stereotactic radiosurgery, but this will offer a different therapeutic endpoint. With surgical removal, the tumor will potentially be cured, whereas radiation, if successful, will only arrest growth and in some cases shrink the tumor. However, surgery is always necessary for larger tumors that are causing dangerous pressure on the underlying brain. Radiation as a stand-alone treatment is contraindicated in such situations as it does not remove the dangerous pressure that the tumor is imparting to the brain and in fact can make it worse by causing the tumor to swell.
Large meningiomas can be time-consuming to remove, with surgery frequently taking 10 or 12 hours or longer.
The objective of meningioma surgery is to return the patient to a normal life with as few complications as possible. In complicated situations, this may mean sacrificing total removal for near-total removal with sparing of vital structures.
Example
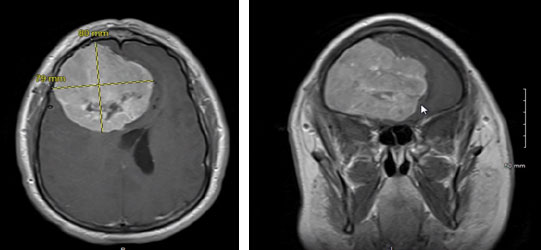
This patient came to attention with headaches and behavioral changes. There was a change in personality with combativeness, short temper, and irritability that resulted in loss of employment due to disruptiveness. This tumor is 8 cm in its greatest dimension and was exerting critical pressure causing compression and shifting of both frontal lobes of the brain which produced the symptoms reported.
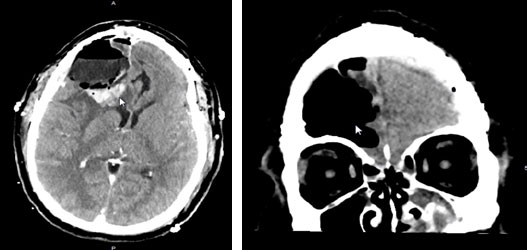
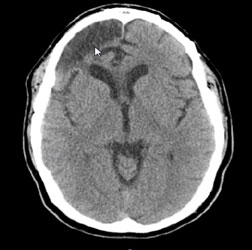
Post-operative CT imaging shows complete resection of the tumor. The arrow on the left image shows a thin layer of postoperative blood in the posterior portion of the resection cavity. The arrow in the imaging on the right points to the cerebrospinal fluid-filled tumor resection cavity which will diminish in size over time as the brain slowly re-expands from the chronic pressure the tumor exerted on it. With very large tumors, there will typically be some residual deformation of the brain that remains permanently as a consequence of the chronic pressure that for years deformed the normal brain. This is seen in the image below where the arrow points to the edge of the re-expanded right frontal lobe, with the spinal fluid just anterior to this in the area of where the chronic pressure altered the shape of the underlying brain. This image is taken 4 years after the microsurgical resection of the tumor, and there is no sign of recurrence on this imaging. The patient's personality returned to normal with the exception of a slight tendency to impatience, and he otherwise lived a normal life.
Below is a photograph of a very small meningioma that was superficial and able to be removed in one piece. Most often, large meningiomas are reduced in size by debulking the center of the tumor first. Then the sides of the tumor that interface with the brain can be carefully dissected from the adjacent brain tissue. This minimizes the need to retract and manipulate the brain. Some meningiomas are soft and rubbery like the one below, while others are dense and fibrous. Some can be very densely calcified. Some may be filled with tumor blood vessels. Some of these characteristics can slow down the process of surgical removal.


 Hablamos Español
Hablamos Español